A 61 year old patient with complaints of fever,SOB and cough since 5 days
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box is welcome.
Here is a case i have seen:
61 year old male farmer by occupation and a resident of nakrekal got married 40years ago.His wife is a home maker.He has three children,two daughters who got married and a younger son got married and working as a farmer.Patient used to do his daily activities and farming since diwali 2019.Post diwali patient was complaining of generalised weakness,SOB and palpitations while doing his manual labour work.patient had been home since then.
H/O deviation of mouth to right side was present since ?10years and left side ptosis present and loss of wrinkling on left side(?Left side Bell’s palsy)Patient and his attenders did not give much attention to it since there was no limb weakness,difficulty in speech or swallowing.No other complaints
Post diwali in 2019 patient was complaining of generalised weakness,SOB and palpitations while doing his manyal labour work.patient had been home since then.
Patient was apparently asymptomatic 3 months back,then he developed fever for which he was taken to a hospital and was diagnosed with typhoid and treated in hospital,during routine investigations patient attenders were informed that the patient had kidney problem and need further evaluation.patient was on irregular medications. Later patient had fever on/off and decreased urine output,generalised weakness, was taken to a local hospital and referred here in view of raised creatinine.
Patient presented with complaints of SOB since 5 days, fever since 5 days and cough since 5 days.
Fever - lowgrade,intermittent,reduced on medication
H/0 SOB since 5 days (grade 3)
Cough with sputum since 5 days sparse in quantity,non blood stained
K/C/O CKD since 3months and on conservative management
Not a K/C/O DM,HTN ,TB ,Epilepsy,CAD,
H/o alcohol consumption for 25 years,stopped 1 year back,consumed toddy and 180ml of whisky
H/O smoking-(chutta) for 15years, stopped 10years back
O/E: pt is conscious,coherent and cooperative
BP- 130/80mm Hg
PR- 98 bpm
RR- 28cpm
Cvs -S1S2 present.
RS-
Inspection - Shape of chest elliptical and bilaterally symmetrical .
No dropping of shoulder
No visible apex beat .
No shifting of trachea .
No scars ,sinuses ,no kypho scoliosis.
Palpation -
Trachea is in midline .
Apical impulse felt in left 5th intercostal space in mid clavicular line .
Decreased chest expansion on left side .(Anterior ,posterior and upper thoracic movements.)
Decreased vocal fremitus on left MA ,SCA ,ICA,ISA,inter scapular areas. IAA ,SSA .
PERCUSSION:
Stony dullness present on left side - MA,AA,IAA ,SSA,ISA.
AUSCULTATION:
— Decreased breath sounds on left Inter SA,Infra SA,AA,IAA,MA
—crepts heard in right InfraSA,AA,IAA
P/A- soft,non tender
CNS-
Loss of forehead wirnkles on left side
Difficutly to close his left eye
Deviation of mouth to right side.
No other focal neurological deficits .
INVESTIGATIONS:
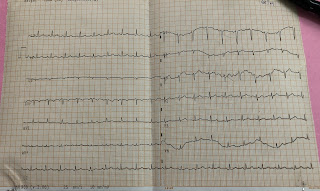
ECG
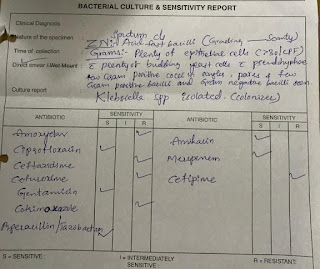
Sputum ZNstaining showing scanty staining
USG-
CHEST X-RAY

PATIENT WAS TAKEN FOR DIALYSIS AT 4:00pm on 8-1-21 ; UF WAS 1lit; SOB DECREASED
UREA DECREASED FROM 223 to 138
Dialysis done on 11-1-21 and ultrafiltrate was 1lit
Dialysis done on 14-1-21 and UF was 1lit
Dialysis done on 17-1-21 and UF was 500ml
TREATMENT:
1-SALT AND FLUID RESTRICTION
2-TAB.LASIX 40mg PO/BD
3-T.NODOSIS 500mg PO/TID
4-T.SHELCAL CT PO/BD
5-T.OROFER XT PO/OD
6-INJ PIPTAZ 2.25gm IV TID
7- BP/PR/TEMP/SPO2 MONITORING











Comments
Post a Comment